Streamline benefit verification and prior authorization workflows by >75%
Plenful's pharmacy-specialized LLMs power the entire end-to-end workflow, from benefit verification to prior authorization, accelerating time to therapy.






















As demand increases, Specialty Pharmacy teams are under increasing pressure to streamline authorization workflows
Complex Therapies Require Complex Coordination
Specialty drugs come with complex payor rules — from formulary coverage to prior authorization criteria — that require teams to gather information scattered across EHRs, payor websites, and portals. Teams spend hours sourcing and reconciling data to determine patient eligibility and meet these requirements.
Prior Authorizations Demand Deep Expertise
Specialty prior authorizations require extensive review of patient history, clinical documentation, and payor utilization criteria. The process is time-intensive and prone to errors — even minor mistakes can lead to delayed therapy.
Fragmented Data Limits Financial Oversight
Performance, reimbursement, and productivity data live in disconnected systems, leaving specialty pharmacy leaders without visibility into team efficiency or margin impact. Without centralized insights, it’s nearly impossible to develop key strategies, track financial performance, or scale operations.
Faster Authorizations. Smarter Workflows. Better Care.
Plenful’s AI-powered benefit verification and prior authorization solutions automate the complexity of specialty pharmacy operations — connecting data, reducing manual touchpoints, and accelerating patient access to therapy.
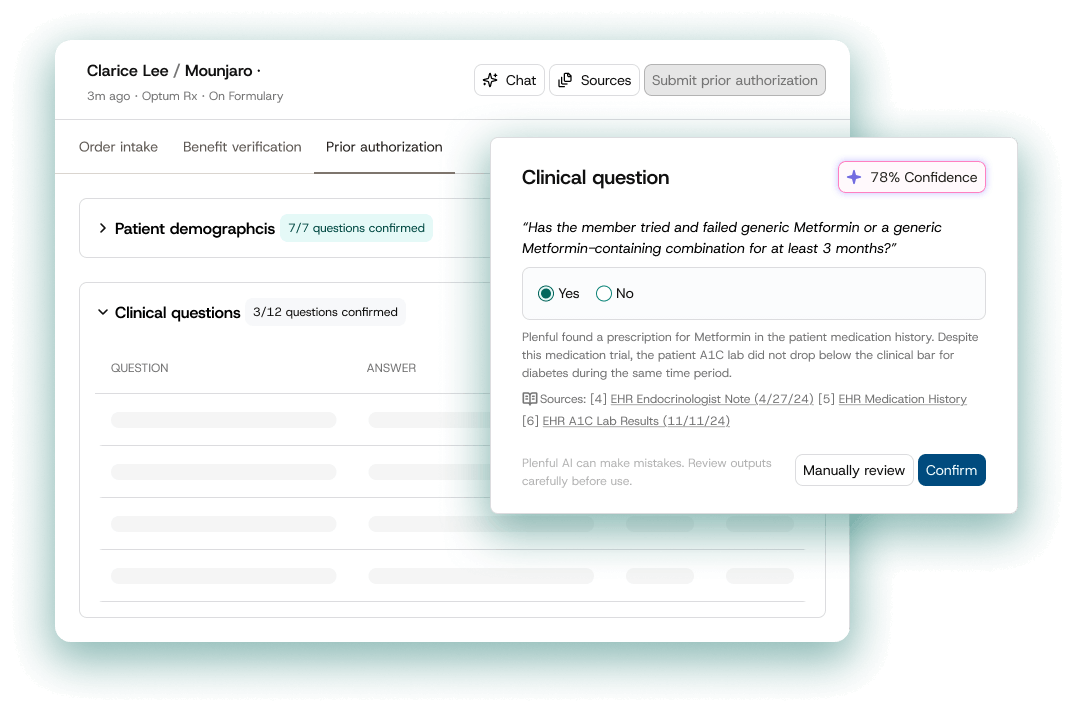
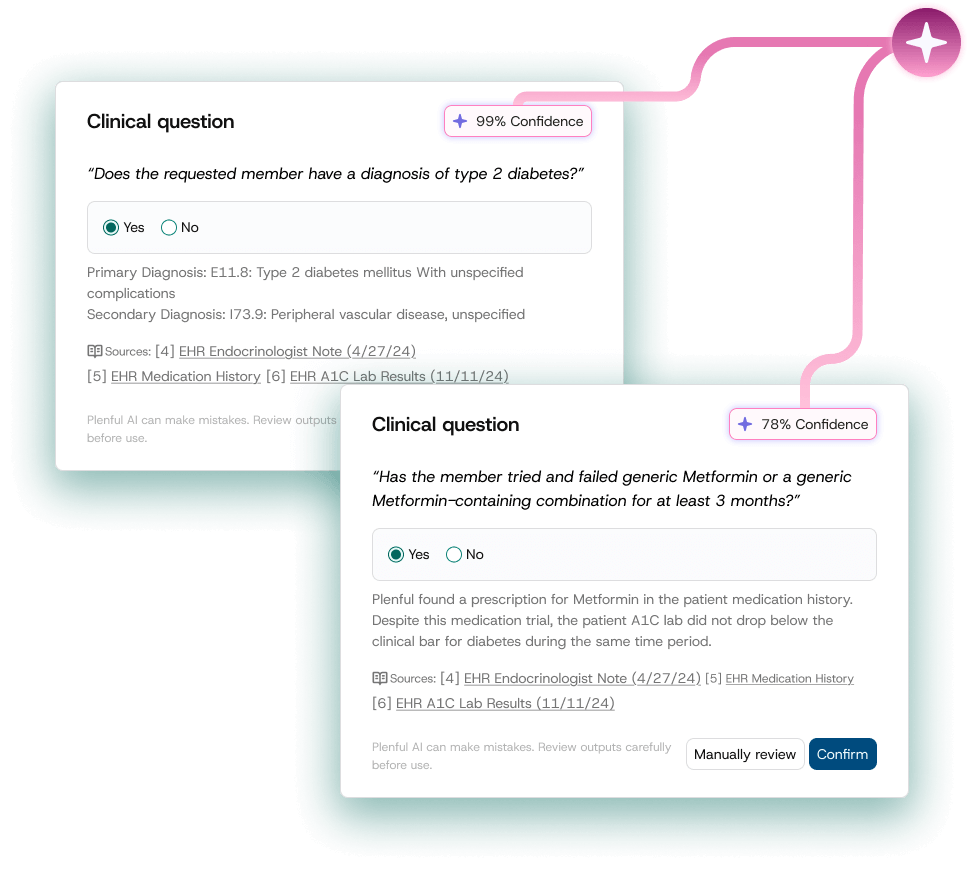
Intelligent Prior Authorization
Plenful’s large language models (LLMs) read and understand complex patient data, automatically populating prior authorization forms with precision and context.
Unified Workflow Management
Manage all benefit verification and authorization workflow from a single platform — no more jumping between EHRs, spreadsheets, and payor portals.
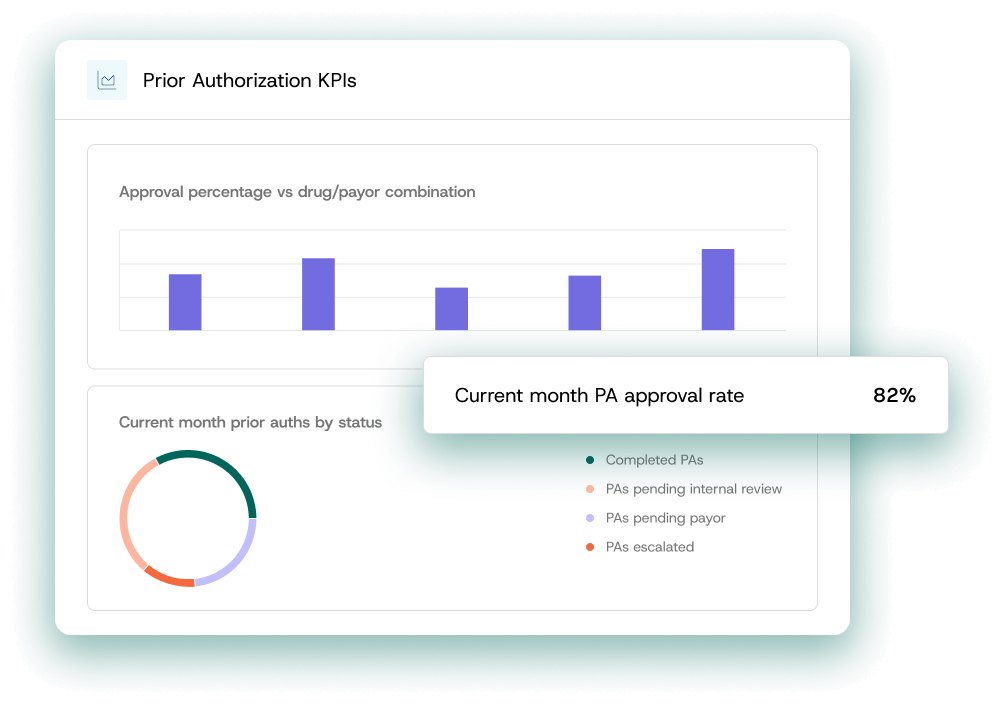
Real-Time Visibility & Insights
Track turnaround times, approval rates, and payor details with dashboards built for specialty pharmacy leaders. Make data-driven decisions to scale your pharmacy operations with confidence.
Plenful cuts Specialty Pharmacy authorization time by 75%, freeing teams to focus on patient care
Automate Benefits Verification
Plenful automates checks for insurance benefits and surfaces key plan rules, including formulary and prior authorization requirements.
Streamline Prior Authorizations
LLMs confidently pre-fill complex prior authorization forms using deep reasoning to analyze patient history, payor rules, and provider notes, cutting submission time from hours to minutes. Plenful fine-tunes as the platform learns from your team's adjustments and clinical expertise.
Executive 360 Dashboards
Gain full visibility into performance and productivity metrics, authorizations statistics, and approval rates with configurable dashboards.

Trusted by 85+ Enterprise Healthcare Organizations
"Plenful comes from pharmacy operations, they just get it. Their AI platform has given us the scalable infrastructure we need to handle increasing medication volumes without proportionally increasing our staffing costs. We've been able to streamline our workflows, reduce processing times, and dedicate more time and care to our in-need patient population.”
Adam Porath